Abstract
Background: Measurable residual disease (MRD) has prognostic importance for patients with acute myeloid leukemia (AML) at many stages of disease. Methodology around MRD testing, and how physicians incorporate MRD into routine practice remains undefined.
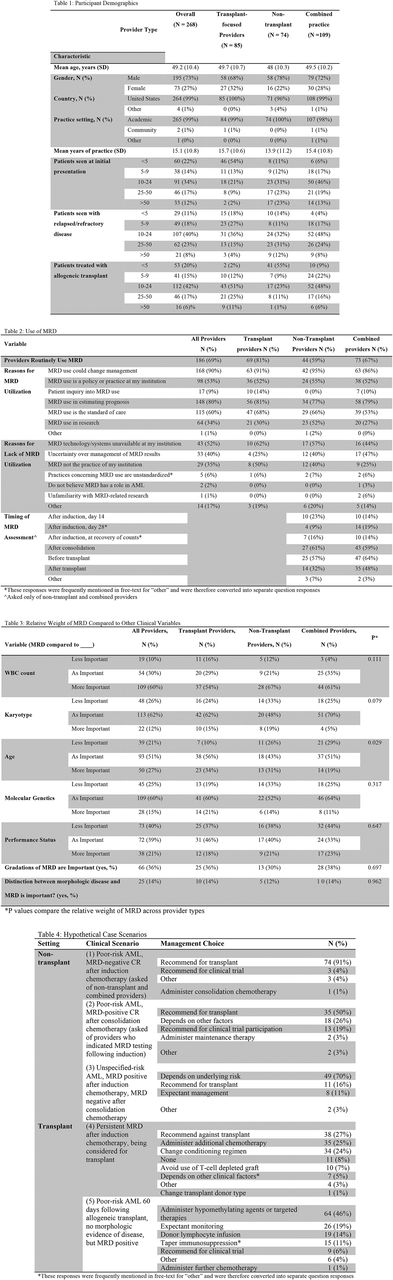
Methods: A survey instrument was developed and distributed to a large international sample of leukemia physicians. Contact information was obtained from the Eastern Cooperative Oncology Group, the Leukemia and Lymphoma Society, and the websites of all 69 NCI cancer centers. Basic demographic information was collected along with details concerning MRD practices, including rationale for its use, its weight against other clinical parameters, diagnostic assays utilized, and its application in theoretical case examples. A multivariable logistic regression model evaluated provider characteristics predictive of MRD utilization.
Results: 268 responses were received (RR = 41%). Table 1 displays provider characteristics. Most providers were men (73%), and in academic practice (99%); median age was 49 years. 69% of providers reported routine use of MRD in management of AML (Table 2), most commonly (90%), for its role in guiding therapy; providers who did not use MRD routinely cited inadequate resources (58%) and uncertainty regarding use of MRD testing results (40%). Female, more experienced, and transplant-based providers were more likely to use MRD in a multivariable analysis. As displayed in Table 3, majorities considered MRD to be more important than WBC (60%), equally important as age (51%), pre-treatment karyotype (62%), and pre-treatment molecular genetics (60%); 40% of respondents regarded MRD as less important than performance status. Providers utilized flow cytometry- more than polymerase chain reaction-based assays (77 vs. 23%), with nucleophosmin-1 being the most common genetic target. In hypothetical case scenarios (Table 4), a majority (91%) recommended allogeneic transplant for an adverse-risk patient who was MRD-negative following induction. In the post-consolidation setting, only 50% would recommend transplant for MRD-positive AML. Among transplant or combined practice providers, for a patient who was otherwise going to be considered to undergo transplant but who was MRD positive after induction, similar proportions recommended against transplant (27%), for giving further chemotherapy (25%), and for altering the conditioning regimen used (24%).
Conclusions: Use of MRD in treating patients with AML was frequent but incomplete in contemporary practice. Providers utilized MRD primarily in making treatment decisions and in estimating prognosis, but lacked uniformity in these practices. Standardization of assays, adoption of requisite technology, and dissemination of data about the value of MRD use would likely increase usage of MRD in the care of patients with AML.
Stein: Seattle Genetics: Research Funding; Novartis: Consultancy, Research Funding; Agios Pharmaceuticals, Inc.: Consultancy, Research Funding; Pfizer: Consultancy, Other: Travel expenses; Constellation Pharma: Research Funding; GSK: Other: Advisory Board, Research Funding; Celgene Corporation: Consultancy, Other: Travel expenses, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal